Click here for a full transcript.
Back in 1975, Polly Murray had been to doctor after doctor, trying to figure out what was happening to the children of Lyme, Connecticut.
Why did it take so long to figure out Lyme disease?
Science is, by definition, slow. It’s easy in 2019 to look back and say, well duh, Lyme disease is spread by ticks and is treated with antibiotics. But back in 1975, when researchers were first investigating the disease, they had to rule out all the possibilities. They had to check water supplies, investigate the local schools, collect and test mosquitoes, and count ticks, one by one.
To study a novel disease, you have to focus on something objective like symptoms that can be measured, tested, or observed with the naked eye. This is called a case definition. It’s incredibly important because a case definition outlines and focuses an epidemiological investigation so that it doesn’t go off the rails. Researchers start with the narrowest case definition possible, and work their way outwards.
Dr. Allen Steere (Yale archives)
Dr. Allen Steere is one of two doctors whose work is most commonly associated with Lyme disease today. Today, Dr. Steere is a researcher and professor of rheumatology at Harvard but back in 1975, he had just finished up two years with the Disease Detectives - The Epidemic Intelligence Service- and was starting a fellowship in rheumatology at Yale when he received a call about what was happening in Lyme with the large number of cases of Juvenile Rheumatoid Arthritis (JRA).
Dr. Steere began looking for children with JRA. He met with the school nurse and local doctors, and he met with Polly Murray.
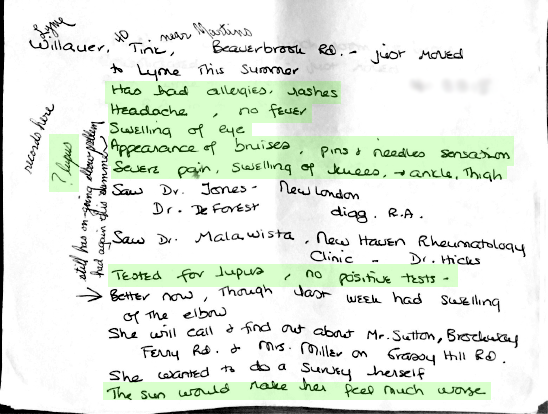
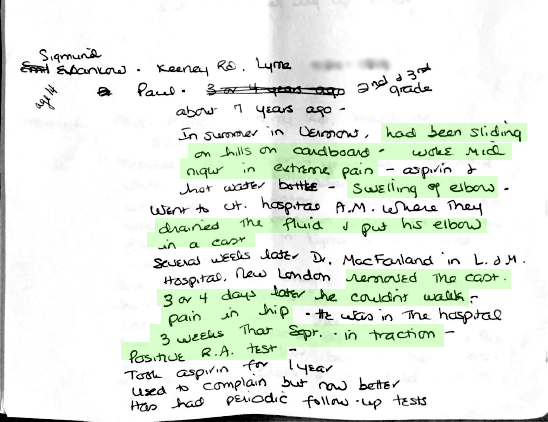
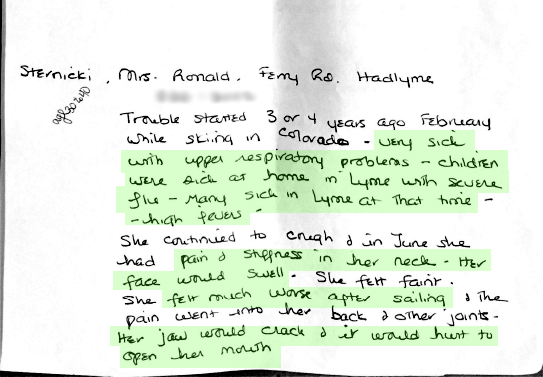
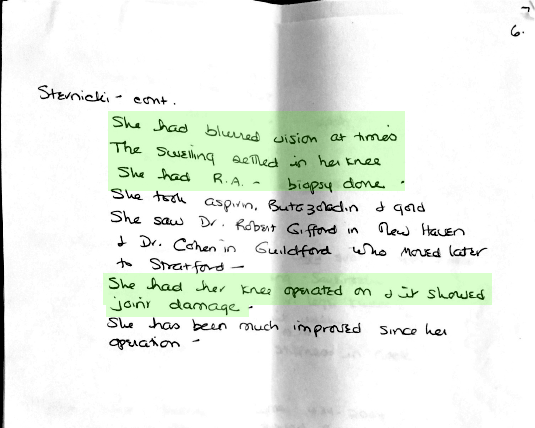
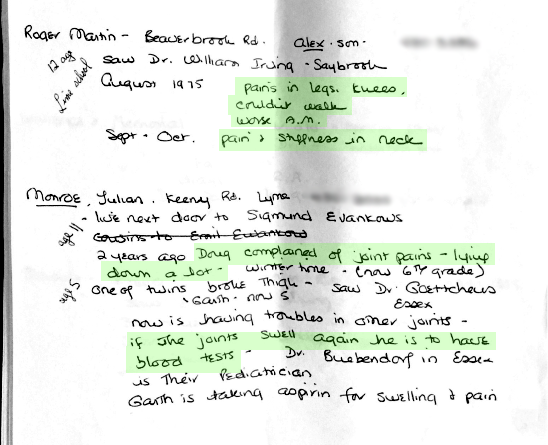
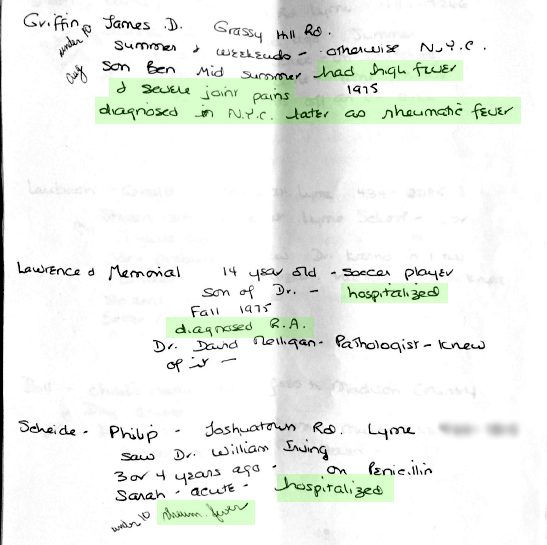
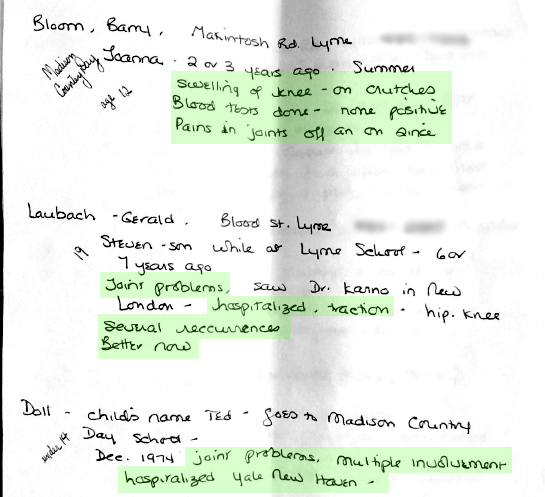
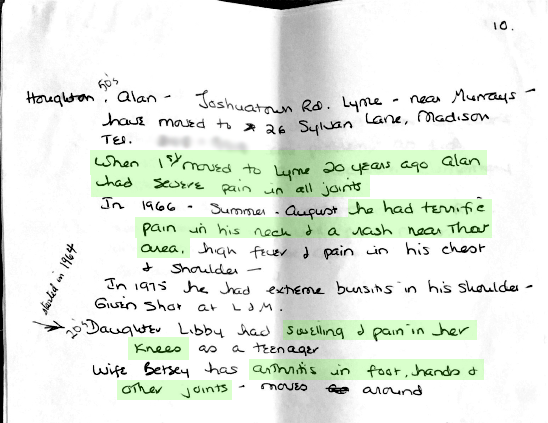
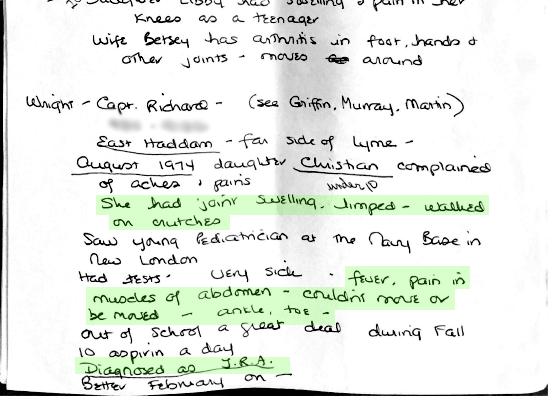
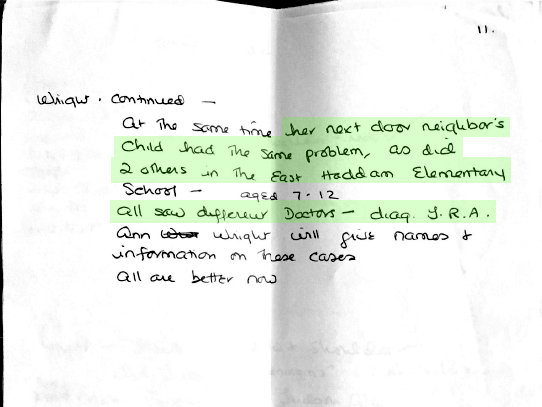
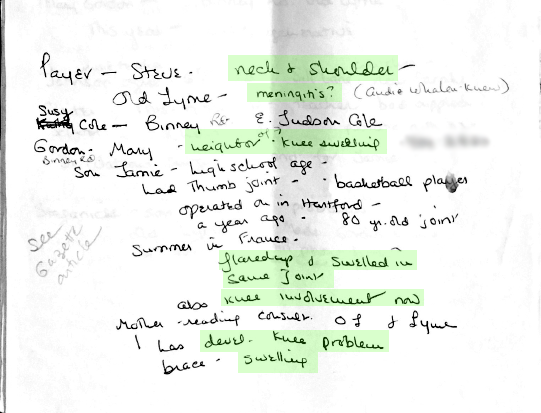
Polly Murray had come prepared when she met with Dr. Steere. She’d been documenting her family’s health for years but over the past few months, she had become a veritable amateur epidemiologist interviewing neighbors and parents, conducting her own miniature investigation. She had names and contact information.
Above: Some of Polly Murray’s notes about others in her area experiencing similar symptoms. Phone numbers have been obscured.
But Dr. Steere was looking for children with arthritis and many of the contacts she provided did not qualify for Steere’s study. In fact, Polly herself did not qualify. Two of her sons did but her own symptoms were stranger and harder to pin down.
Dr. Steere began his investigation in December 1975. The following May, he wrote to participants about his as-of-yet unpublished findings: 39 children and 12 adults met their criteria, most of whom suffered bouts of arthritis, especially in the knees, preceded by a flu-like illness some time before.
There were other strange symptoms reported too - nerve pain, facial paralysis, trouble sleeping - but these were inconsistent, not as easily defined, and by design not the current focus of the investigation.
Science is compartmentalized by necessity. There’s too much to learn, so experts have to focus that knowledge in order to make progress.
Steere was a rheumatologist, so he focused on the one thing he knew best. He called the unknown disease Lyme Arthritis. He believed it was caused by a virus and that it would get better on its own, like the flu. He advised patients to treat pain and swelling with Aspirin.
At the same time, Yale scientists were collecting tens of thousands of mosquitoes and thousands of ticks as well, searching for the pathogen that might be causing Lyme Arthritis. Dr. Steere speculated that mosquitoes might be the cause.
But Dr. Steere’s theory was wrong: often, Lyme disease does not go away on its own, and it is not treated with aspirin. But that’s science. Steere was making an educated guess. And it didn’t pan out. But that’s science.
A few years later, the Yale researchers released a statement. They were no longer studying Lyme Arthritis; they were studying Lyme Disease, a multisystem illness that could invade the joints, the heart, the facial nerves, and the lining of the brain.
They had collected enough evidence to widen the case definition, and confirm what Polly Murray had believed all along - that the disease was more serious than originally thought.
And after years of recommending aspirin, they changed course. They started recommending antibiotic treatment for patients with a bullseye rash and unusual bouts of arthritis, but they didn’t know for sure which type of antibiotic was best, or for how long.
One thing was certain, though: Lyme disease wasn’t being spread by mosquitoes. Cases were coming from a number of states, roughly matching the geographic range of what we now call the blacklegged tick.
(Sara Plourde, NHPR)
Across the country in a lab in Montana, microbiologist Alan Barbour and medical entomologist Willy Burgdorfer found something unusual inside a batch of ticks from Long Island, New York: a spirochete.
Borellia burgdorferi, the spirochete responsible for Lyme disease (CDC Public Health Image Library)
A spirochete is bacteria that twists like a corkscrew. The most famous spirochete is the one that causes syphilis. But neither Barbour nor Burgdorfer recognized this one. They ran some tests and eventually managed to isolate the bacteria. It was an unknown pathogen, the causative agent of Lyme disease. They named it Borrelia burgdorferi, after Willy Burgdorfer.
In the years after the bacteria was identified, Polly Murray was invited to scientific conferences to speak about her experiences in Lyme. She collected piles and piles of medical journals and scientific papers about the disease.
In 1975, 51 people in Connecticut were diagnosed with what would later be known as Lyme Disease. Today, it’s the most common vector-borne disease in the United States.
But what exactly is the disease doing when it gets into your body? A trip into the tick and your body in episode 3.
SCIENCE EXTRA
Scientists at the Cary Institute for Ecosystem Studies in Millbrook, New York, have been studying the relationships between ticks, white-footed mice, and Lyme disease for decades.
They take samples of tissue, blood, urine, and feces, and count all of the ticks on every mouse they catch.














This is what science looks like: four people, sitting in white coveralls at a plastic poker table in the middle of the woods, counting ticks with tweezers.
All day. Every day.
This is the actual pace of the epidemiological progress, too, which is easy to forget when you’re the one waiting for answers.
(Photos by Taylor Quimby, NHPR)